The prostate is the most common cause of health problems that men face over the course of their lives. There are many treatments now available - the majority not involving surgery. So men should seek help and have a PROSTATE CHECK!
The Anatomy
The prostate is a small, almond-shaped gland that sits at the base of the bladder. Its main function is to produce the majority of fluid that a man ejaculates, but it is not essential for life.
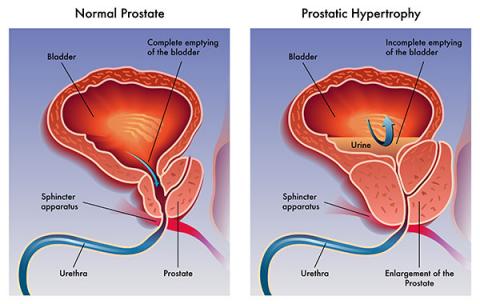
It enlarges throughout a man’s life, and can commonly cause problems with a man’s “waterworks”. As can be seen from the diagram the urethra passes through the middle of the prostate, and as it grows it compresses this tubular structure. This compression in turns leads to the difficulty men often experience in passing urine as they get older.

Basic Terms used when talking about the prostate and the urinary tract
-
Micturation – the process of passing urine, also known as urination.
-
Lower Urinary Tract Symptoms (LUTS) - the common term used to refer to symptoms from the prostate.
-
Frequency – the need to pass urine often.
-
Nocturia – the need to get up at night to pass urine.
-
Dysuria – a “burning” feeling in the urethra when passing urine.
-
Benign Prostatic Hyperplasia (BPH) – the normal enlargement of the prostate that most men experience.
-
International Prostate Symptom Score (IPSS) – a simple questionnaire about your symptoms.
-
Digital Rectal Examination (DRE) – Examination of the prostate.
-
Mid Stream Urine (MSU) – standard urine pathology test to look for infection.
-
Full Blood Count (FBC).
-
Urea, Electrolytes, Creatinine (U / E / Cr) – these are the standard renal (kidney) function tests.
-
Prostate Specific Antigen (PSA) – a blood test designed to help in the diagnosis and management of prostate problems, including cancer.
-
U/S (or US) – Shorthand for ultrasound.
Common Symptoms
Symptoms caused by problems with the prostate are often known collectively as “lower urinary tract symptoms” or LUTS.
Symptoms and signs of prostate problems include:
-
A delay before starting to pass urine – hesitancy.
-
Poor stream – slow, may stop and start.
-
The need to strain to keep the urine flowing.
-
Passing urine often – frequency.
-
Needing to pass urine at night – nocturia.
-
The need to rush to pass urine urgently – urgency.
-
Dribbling urine onto the underpants after finishing urination – post-micturition dribbling.
-
Burning pain when passing urine – dysuria.
LUTS (lower urinary tract symptoms) are rarely caused by cancer, though when you are investigated, the Urologist will often seek to exclude this possibility (more later). The most common prostate problem that causes these symptoms is BPH (Benign Prostatic Hyperplasia).
BPH occurs in all men - prostates enlarge throughout adult life. The size of the prostate does not correlate well with the occurrence of symptoms. Many men with large prostate have few symptoms, whilst conversely some men with small prostates may experience quite severe LUTS.
The diagram demonstrates how the prostate can block the bladder (BOO = Bladder Outlet Obstruction) as it enlarges. Treating the prostate for enlargement does not result in incontinence, as the prostate sits above the urinary sphincter and is separate from that structure.
The Diagnosis - how is it made?
You will find that some or all of the following may be required to make an accurate diagnosis of LUTS caused by your prostate:
-
History – your medical history, including medications, past problems or previous surgery.
-
IPSS – a simple questionnaire that can help evaluate the severity of your symptoms, and your response to any treatment. You can download an IPSS to assess yourself (bring it to your consultation if you like).
-
Examination – especially a DRE (digital rectal examination). The abdomen and genitals are often examined as well.
Digital Rectal Examination

The rectal examination should NOT cause you any anxiety. It is not painful (though perhaps a little embarrassing). It is performed with you lying on your left side or alternatively whilst standing and bending over with your elbows on the examination couch. Most people find the latter method more comfortable (or perhaps less uncomfortable!) This examination allows the doctor to obtain an indication of the size of your prostate as well as the presence of any lumps or nodules, etc.
-
Urine tests – to look for infection, blood, sugar etc.
-
Blood tests – general blood count and kidney function tests.
-
PSA – Prostate Specific Antigen. This is a useful test to help the doctor manage your prostate problem. It can be an indicator of underlying cancer, though it is not a test that is specific to prostate cancer. Feel free to discuss this test with you doctor. Visit Andrology Australia website for more information on PSA.
Other Investigations
You may be required to have one or all of the following tests as well:
-
Ultrasound – to image the kidneys and bladder.
-
Post-Void Residual – usually performed at the same time as the ultrasound. This test measures how much urine is left in your bladder after you pass urine.
-
Cystoscopy – telescopic inspection of the prostate and bladder.
-
Urodynamic study – a computer based test of you bladder function.
Treatment Options
There are many treatment options for BPH that do not involve surgery. Once
“dangerous” conditions such as prostate cancer, bladder cancer, kidney disease, bladder stones etc. have been excluded, the need for any treatment depends on how bothered you are by your LUTS. You will have noticed the so-called bother score you provided if you completed an IPSS questionnaire. Some of the treatment options are listed below:
Risks
The main risk men face when suffering from LUTS due to prostatic enlargement is acute urinary retention. This is the medical term for when a person cannot urinate - they usually suffer severe pain and need to go to hospital to have a catheter inserted in the bladder.
The other risks faced are urinary tract infections and more rarely kidney failure and bladder stones.
What you can do for yourself - lifestyle changes

You may decide you do not wish any specific medical treatment at this point in time. Some of the following tips may help make some of your symptoms more bearable:
-
Drink a little less fluid in the evening.
-
Some drinks such as tea, coffee and alcohol can exacerbate the symptoms.
-
Some medications (such as diuretics) make you pass more urine - a consultation with your local doctor may enable these drugs to be taken in the morning.
-
“Urethral milking” – after passing urine run your finger from behind the scrotum forward to push out those last few drops of urine that often stain the underwear.
-
“Herbal” remedies that can be bought over the counter can often improve symptoms e.g. Saw palmetto.
-
Sometimes pelvic floor exercises help - download a pamphlet if you like (or ask for one).
-
You should have an annual prostate check as back-up to ensure you are not developing any hidden problems.
Medications
If your symptoms are causing you a moderate amount of bother you may elect to try some of the available medications.
Alpha Blockers

These drugs block the nerves to the muscles of the prostate. This relaxes the prostate and allows easier passing of the urine. Symptoms improve 2-4 weeks after commencing the drugs. Prazosin (Minipress or Pressin) is relatively nonspecific and in larger doses is used as a blood pressure tablet. Its big advantage is that it a PBS listed drug. Tamsulosin (Flomax) a prostate-specific alpha-blocker that works more rapidly and often with more effect, but at this time is only on the Repatriation PBS scheme - therefore for most people it costs about $50 per script.
5 Alpha-Reductase Inhibitors

These drugs - the two available in Australia are Finasteride (Proscar) and Dutasteride (Avodart) - reduce some of the hormonal activities of testosterone in the prostate causing it to shrink. These drugs have proven to be highly successful in helping men with an enlarged prostate.
Combination Therapy
As you have probably already surmised combining an alpha blocker with a 5 Alpha Reductase Inhibitor would not only relieve symptoms but prevent further growth of the prostate (even shrink it) and thus prevent the development of the possible side effects of prostate enlargement such as urinary retention, renal failure and surgery. This has in fact been done and proven to be a highly successful strategy in a man suitable for such therapy. A combination pill (Duodart) with both Tamsulosin and Duatsteride inside is available in Australia on the PBS i.e. normal script price.
Surgical Options

When your symptoms are severe, you do not respond to medication, or the prostate enlargement is putting you at risk, then surgical options may need to be explored. Your Urologist will explain these in detail.
Options range from the minimally invasive to open surgery (though this highly unlikely to be required these days). Possible surgical options include:
-
Urolift Procedure – the obstructing prostate tissue is “pinned” open to relieve symptoms.
-
TURP – traditional endoscopic (no cuts) removal of the central part of the prostate. This is the basic operation that all the laser forms of surgery attempt to emulate e.g. Greenlight laser, Holmium, etc.
-
Laser TURP – uses laser energy to remove or ablate the obstructing prostate tissue. Main advantage is that the operation can be performed using Saline, which decreases the chance of some of the possible complications.
-
Open Prostatectomy – involves formal surgical removal of the inner prostate (i.e. an old fashioned style of operation) - highly unlikely to be these days.
